A popular Facebook post in August 2020 was not alone in taking issue with one estimate concerning the COVID-19 virus’ mortality rate, but might also mislead readers looking for an easy answer.
The post, first published on August 20, 2020 and shared more than 14,000 times since, calls reports that the virus has a 0.04 percent death rate “dead wrong”:
To get an accurate death rate for the disease, you divide the deaths by the total cases that HAVE AN OUTCOME. Let’s walk this through.
As of right now, there are 5,671,984 COVID cases in the US. 175,617 people have died because of COVID. 3,028,393 people have recovered.
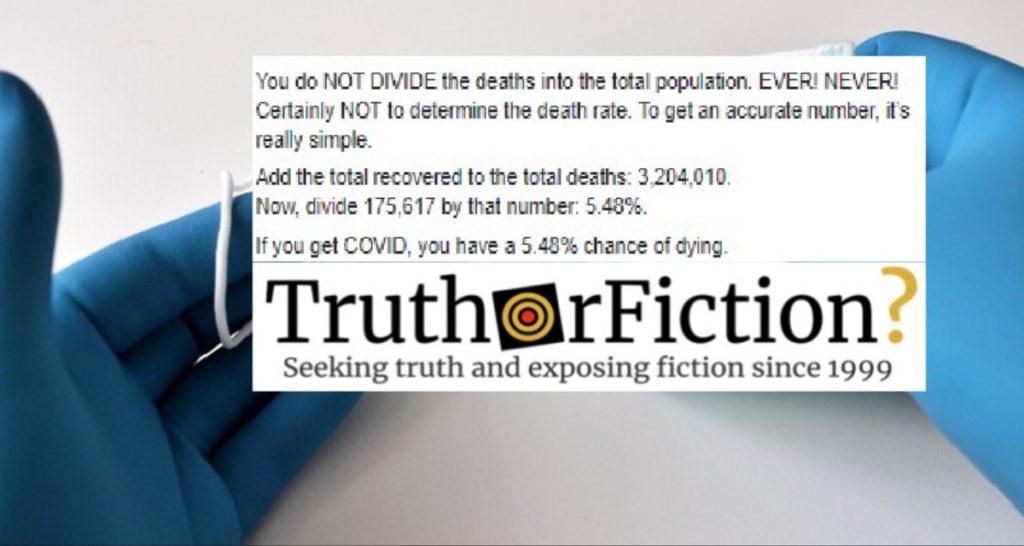
You do NOT DIVIDE the deaths into the total population. EVER! NEVER! Certainly NOT to determine the death rate. To get an accurate number, it’s really simple.
Add the total recovered to the total deaths: 3,204,010.
Now, divide 175,617 by that number: 5.48 percent.
If you get COVID, you have a 5.48 percent chance of dying.
By comparison, Influenza has infected around 39,000,000 people this last season, with around 50,000 deaths. That’s a 1.28 percent death rate.
You are five times more likely to die from COVID if you get it than you would if you got the flu. It’s not the flu. It’s not even a cold.
Dr. Stephen Kissler, a research fellow for the Department of Immunology and Infectious Diseases at Harvard University, told us that calculating the death rate for COVID-19 is not as simple as the post makes it out to be. While it is easier to determine posthumously whether someone was killed because of the virus, researchers “probably have a very big underestimate” of how many COVID-19 cases have actually ocurred.
“If we were to adjust the number of COVID-19 cases that were cited in that graphic to reflect what we think is probably closer to the true number, then we’d be dividing the same number of deaths by a larger fatality number, which would make the infection fatality rate decrease somewhat,” he said.
One factor that can influence calculating the virus’ infection fatality rate (IFR), Kissler explained, is that COVID-19 does not claim its victims quickly. Because of that, death figures could reflect infections that took effect up to a month earlier.
“You have these opposing forces,” he said. “First, we’re probably undercounting the number of cases that are occurring. But just due to the trajectory of the epidemic itself — that can also cause us to underestimate the infection fatality rate, and that’s why this is so complex.”
The complexity of the issue, Kissler said, is why there have been arguments concerning the virus’ IFR.
The post’s premise that the death rate for the virus has been inaccurately reported as being .04 percent has also been explored independently. The statistic itself originated from a scientific pre-print — a study that has yet to be published or peer-reviewed. As the Associated Press reported, the figure first appeared in a study by Dr. John Ioannidis, a Stanford University professor of medicine.
According to Ioannidis, the infection fatality rate (IFR) for the virus “ranged from 0.00 percent to 0.57 percent” with a corrected median rate of 0.04 percent. He based his findings on the results of twelve separate studies measuring the prevalence of antibodies for the virus in separate population centers.
“At a very broad, bird’s eye view level, worldwide the IFR of COVID-19 this season may be in the same ballpark as the IFR of influenza,” he wrote.
But Ioannidis and his work have come under criticism throughout 2020. In March, he predicted — incorrectly — that around 10,000 people in the United States would die from COVID-19. And in May, Buzzfeed reported that he failed to disclose that a previous pre-print examining COVID-19 antibodies was partially funded by JetBlue Airways founder David Neeleman, who has argued against protective measures like remaining at home during the pandemic.
Similarly, other researchers questioned the methodology Ioannidis employed for his latest pre-print.
“A lot of the included studies had issues, and contradicted evidence from numerous places in the world, making the review itself a bit problematic,” Gideon Meyerowitz-Katz of the University of Wollongong in Australia told the San Jose Mercury News.
Andrew Noymer, an associate professor of public health at the University of California-Irvine, also took issue with the study, particularly because — unlike COVID-19 — the flu is already treatable because of the presence of annual vaccinations.
“Not everyone is susceptible to the flu. Everyone is susceptible to COVID-19,” Noymer told the newspaper. “These flu comparisons are missing the forest for the trees.”
The AP also cited another pre-print in its reporting, a study by researchers at Dartmouth College calculating that the virus’ IFR was “close to zero for younger adults but rises exponentially with age.” That analysis, based on findings from separate types of studies including 15 conducted in “specific locations in Europe and the United States,” estimated an IFR of 0.3 percent for people between the ages of 50 and 59 and 10 percent for those aged 80-89.
The World Health Organization has also disputed comparisons between COVID-19 and the flu:
Mortality for COVID-19 appears higher than for influenza, especially seasonal influenza. While the true mortality of COVID-19 will take some time to fully understand, the data we have so far indicate that the crude mortality ratio (the number of reported deaths divided by the reported cases) is between 3-4 percent, the infection mortality rate (the number of reported deaths divided by the number of infections) will be lower. For seasonal influenza, mortality is usually well below 0.1 percent. However, mortality is to a large extent determined by access to and quality of health care.
Kissler took issue with another claim made in the post — that one should “never” divide the number of deaths by a country’s total population; that statistic, he said, is called the population mortality rate, which covers an entirely different question than the one covered in the Facebook post.
“Whereas the question in the post is basically, ‘What’s the probability of dying given infection with COVID-19?’ the question that you’re trying to answer when dividing deaths by the population is, ‘How bad is this epidemic in this particular location — say, in the United States vs in other countries?'” he said. “That gives you an estimate of how many fatalities there are [and] you’re basically adjusting by the population size.”
As of August 25 2020, the Centers for Disease Control listed 176,617 deaths attributed to COVID-19 in the U.S. and 5,715,567 total cases.
- No Consensus on COVID-19 Death Rate for Those Under 70
- The Infection Fatality Rate of COVID-19 Inferred from Seroprevalence Data
- Stanford Researcher says Coronavirus Isn't as Fatal as we Thought; Critics Say he's Missing the Point
- Assessing the Age Specificity of Infection Fatality Rates for COVID-19: Systematic Review, Meta-Analysis, and Public Policy Implications
- Cases in the U.S.
- Q&A: Influenza and COVID-19 - Similarities and Differences
- JetBlue’s Founder Helped Fund A Stanford Study That Said The Coronavirus Wasn’t That Deadly
- A Fiasco in the Making? As the Coronavirus Pandemic Takes Hold, We Are Making Decisions Without Reliable Data