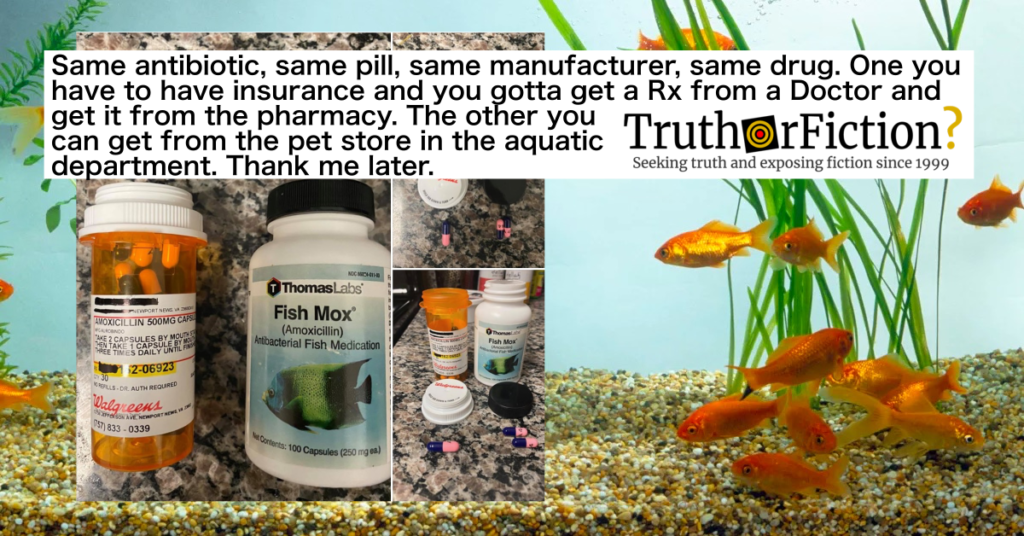
On February 17 2020 a Facebook user shared the following post, claiming that a product called “Fish Mox” is the “same antibiotic, same pill,” and “same drug” as the common antibiotic amoxicillin:
Alongside three photographs, text read:
Same antibiotic, same pill, same manufacturer, same drug. One you have to have insurance and you gotta get a Rx from a Doctor and get it from the pharmacy. The other you can get from the pet store in the aquatic department. Thank me later. ????
A large image to the right showed a prescription of 30 500mg amoxicillin pills (a dose of two capsules), next to a bottle of Thomas Labs “Fish Mox,” 100 capsules of 250mg pills. The second image displayed both bottles open, appearing to contain identical blue and pink capsules. The third showed one pill in front of the open prescription bottle, and two in front of the Fish Mox bottle.
Indeed, the capsules appeared to be identical (assuming the contents of the respective bottles were accurately represented), down to the specific navy blue and pink colored caplets with black markings. What was not clear was whether the pills were indeed correctly labeled, or if the photographs were staged to further the original user’s point.
We contacted our local CVS to ask a pharmacist about the basic claims — whether fish antibiotics were identical to those dispensed by pharmacists. The individual to whom we spoke told us that amoxicillin was not expensive, and we noted that the doctor’s visit to obtain the prescription might be the actual barrier. The pharmacist did not elaborate further, and would only say that CVS did not sell fish antibiotics.
As of the February 2020 post’s spread, the notion of underinsured Americans resorting to using fish antibiotics was not necessarily novel; in fact, it was something of a meme in its own right. As far back as August 2017, Smithsonian Magazine came out with an article warning those who might be in a difficult situation not to risk using fish antibiotics if they were unable to afford a doctor’s visit. A primary reason cited was that fish antibiotics are not expressly regulated by the Food and Drug Administration (FDA) in the same manner as antibiotics or amoxicillin intended for human consumption:
But there are a few key reasons why taking your fish’s drugs is a very bad, no good idea. Let’s start at the top.
First, fish antibiotics are completely unregulated. Technically, they should fall under the purview of the Food and Drug Administration, which oversees both human and animal drugs. Those animals including companion animals (dogs, cats, horses) and food animals (cattle, pigs, chickens). Yet no ornamental fish antibiotics are approved by the FDA.
If a person had a potentially serious infection and no way to access a doctor to obtain a prescription, that particular risk might not be too much of a disincentive. Assuming fish tolerated their antibiotics well and weren’t regularly dying from exposure to the products, humans might deduce Fish Mox was not too risky.
Incidentally, Thomas Labs (maker of Fish Mox) says on their website of their products:
The only FDA registered and inspected fish antibiotic facility offering USP certified quality antibiotics. Quality you can trust.
Another cited reason was that patients are notoriously quick to request antibiotics for viruses and other conditions for which antibiotics are not an appropriate treatment. This behavior in the aggregate can causes antibiotic resistance, rendering common antibiotics less effective, or not effective at all, against once-treatable infections.
Antibiotics are inexpensive — often $5-$10 for a full prescription — and a tempting solution to an illness you can’t seem to shake. According to the World Health Organization (WHO), antibiotic resistance caused by overuse of antibiotics remains “one of the biggest threats to global health, food security, and development today” and “leads to higher medical costs, prolonged hospital stays, and increased mortality.”
That claim related to Smithsonian‘s third point in favor of eschewing fish antibiotics. Namely, antibiotics are typically dispensed by prescription, and a doctor doesn’t usually hand out any old antibiotic, such as the commonly recognized amoxicillin seen in the photographs. The piece noted doctors usually confirm the patient is indeed fighting a bacterial (not viral) infection, and the antibiotics prescribed are one of many used to treat varying types of infection:
When a doctor prescribes you antibiotics, the first step is to make sure you’re dealing with a bacterial infection by running the proper tests. Antibiotics, which are intended to kill or slow the growth of bacteria that cause infection, are useless against a virus—and you don’t want to use them if you don’t have to, or it might lead to bacterial resistance.
The next step is to find out what kind of bacteria you’re up against. Even broad spectrum antibiotics work differently to target different kinds of infections. Moxifish, for instance, contains amoxicillin, a type of penicillin. When a fish absorbs this compound through their skin, it travels through the bloodstream until it latches onto a bacteria’s rigid cell wall. There, it interferes with wall-building, leading to a build-up of pressure that eventually causes the the cell to burst. Unfortunately, many types of bacteria have grown resistant to penicillin: Staphylococcus Aureus, the bacteria commonly responsible for skin infections no longer responds to this class of antibiotics.
As such, consulted experts said, patients could cause more harm to themselves by selecting the wrong antibiotics on Amazon or Chewy:
So what if you skip the doctor, take a gamble and choose wrong? Well, each drug comes with its own set of potential side effects and allergic reactions. Taking amoxicillin while suffering a viral infection such as mono, for instance, can cause the body to erupt in rashes, says Morgan. Ciprofloxacin, previously a go-to for UTIs and sinus infections, has come under recent scrutiny for causing lasting damage to tendons, muscles, joints, nerves and the central nervous system. Many other antibiotic classes come with their own unpleasant effects.
And even choosing correctly doesn’t guarantee success … antibiotics kill off both good and bad bacteria. That means that, to avoid unwanted side effects, it’s crucial to take them for the proper amount of time. Ending an antibiotic regimen too soon—or taking one for too long—can both breed further bacterial resistance. Stop too soon and you risk relapse, potentially allowing the microbes causing the disease to proliferate and form resistance.
In December 2019, study authors presented research on the prevalence and risk of humans using fish antibiotics at the ASHP (American Society of Health-System Pharmacists) 54th Midyear Clinical Meeting & Exhibition in Las Vegas. A brief summary of the presentation and presumably upcoming study reiterated some of the concerns raised in the 2017 article quoted above, mainly concerning doctor/pharmacist oversight and compliance in completely a course of antibiotics:
“While human consumption of fish antibiotics is likely low, any consumption by humans of antibiotics intended for animals is alarming,” [study co-author Brandon Bookstaver, PharmD, director of residency and fellowship training at the University of South Carolina College of Pharmacy] said, in a prepared statement. “We were particularly concerned that the high volume of positive feedback on the comments about human use might encourage others to attempt to use these drugs.”
Fish antibiotics are currently available over the counter, ranging in prices from $8.99 for a bottle of 30 capsules of amoxicillin to $119.99 for a bottle of 100 ciprofloxacin tablets.
The researchers also obtained and examined 5 antibiotics that were being marketed online for fish: amoxicillin, penicillin, cephalexin, metronidazole, and sulfamethoxazole. These products carry the exact imprints, color, and shape of available products meant for human consumption.
Pharmacists can play a critical role in helping patients access safe and appropriate medications, and in educating people about the dangers of taking antibiotics not prescribed to them, according to ASHP Director of Pharmacy Practice and Quality Michael Ganio, PharmD, MS, BCPS, CPHIMS, FASHP.
“What might seem like a less expensive, easier way to treat an assumed infection can ultimately have very serious negative consequences,” said Ganio, in a prepared statement. “Unlike antibiotics for humans or other animals, these medications are completely unregulated by the Food and Drug Administration. Even if the pills look the same, it’s impossible to know that medications purchased in this manner contain what the label says and are safe for humans. Antibiotics, like all medications, should be dispensed from a licensed pharmacy after a diagnosis and prescription from a medical professional.”
Emphasized above is a portion indicating that researchers observed the five “products carry the exact imprints, color, and shape of available products meant for human consumption.” It wasn’t immediately clear if the researchers meant the products were visually identical (thus confusing prospective patients), or if they were saying the products were literally the same exact pills dispensed in pharmacies. (We were unable to find the study itself, suggesting that publication was still pending as of February 2020.)
The summary’s final sentence suggested the former, not the latter was true:
The authors of the study plan to verify the contents of the antibiotics as a next step in their research.
Bookstaver also emphasized concerns about antibiotic resistance:
“While human consumption of fish antibiotics is likely low, any consumption by humans of antibiotics intended for animals is alarming,” Bookstaver said. “Self-medication and the availability of antibiotics without healthcare oversight might contribute to increasing antimicrobial resistance and delayed appropriate treatment. We were particularly concerned that the high volume of positive feedback on the comments about human use might encourage others to attempt to use these drugs.”
Concerns notwithstanding, it was also clear a segment of the population felt they had no choice but to risk using antibiotics for fish and animals due to a lack of health care access. In August 2017, Mashable spoke to many users of fish antibiotics about the reasons they used the medications:
Even with insurance, Carrera Howie couldn’t afford a visit to the doctor. Her mother recommended she take fish antibiotics, and gave her a bottle that she’d purchased from a pet store. She said she didn’t know where the idea originated from.
“They worked incredibly,” she told Mashable in an email. “The UTI was completely gone within a week and I didn’t get another one for at least 4 more years.”
She even said she’d use them again.
“Urgent care and doctors’ copays are so expensive and it sometimes feels like I have to make a choice between having a provider and having groceries,” she explained.
37-year-old Amy Wareham has also turned to fish antibiotics more than once to help cure an illness.
Wareham said went 10 years without insurance, and used fish antibiotics four times during that period to self-medicate. At the time, she compared the pills to pills her family members had gotten from the pharmacy, and claimed that they were identical.
Today, she has health insurance under the Affordable Care Act, and said she wouldn’t use fish antibiotics again — unless she became uninsured.
A viral Facebook post that claims people without access to healthcare have used fish antibiotics for infections is neither unknown nor a major secret. As for whether the medications are genuinely identical. that is truly unknown. Researchers are currently testing fish antibiotics alongside those manufactured or marketed for human consumption. Doctors and pharmacists asked about the safety of fish antibiotics cite mainly concerns over FDA oversight of the pills, as well as the risk of inaccurate or complete antibiotic courses and a larger risk of contributing to antibiotic resistance.
- This Is Why Taking Fish Medicine Is Truly a Bad Idea
- Thomas Labs®
- Home/Newsroom/Fact sheets/Detail/Antibiotic resistance
- Study: Human Consumption of Fish Antibiotics May Lead to Dangerous Consequences
- Human Consumption of Fish Antibiotics Investigated in New Study
- Meet the people using fish antibiotics as a cheap alternative to American healthcare