On August 29 2023, a tweet about disabled people and Medicaid-related laws about cash and assets was shared to Reddit’s r/facepalm:
The Post and the Original Tweet
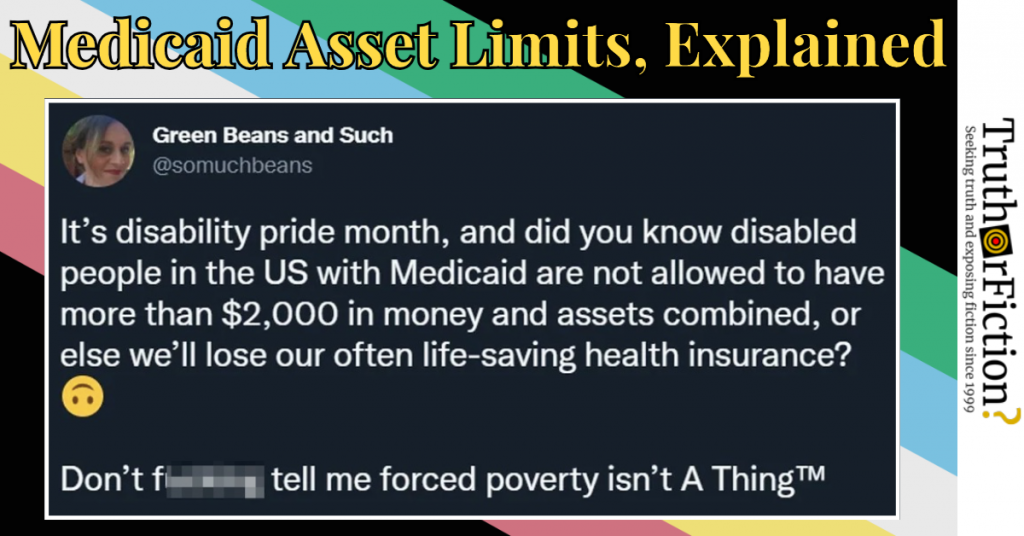
A screenshot of a tweet appeared alongside the post (“I didn’t know that, yeah.”) It was attributed to Twitter user @somuchbeans:
Fact Check
Claim: “It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than
The Post and the Original Tweet
A screenshot of a tweet appeared alongside the post (“I didn’t know that, yeah.”) It was attributed to Twitter user @somuchbeans:,000 in money and assets combined, or else we’ll lose our often life-saving health insurance?”
Description: A viral tweet claimed that during Disability Pride Month, disabled Americans enrolled in Medicaid are not allowed to have more than
The Post and the Original Tweet
A screenshot of a tweet appeared alongside the post (“I didn’t know that, yeah.”) It was attributed to Twitter user @somuchbeans:,000 worth of combined money and assets, or they risk losing their health insurance.
It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ????
Don’t fucking tell me forced poverty isn’t A Thing™
No date was visible on the screenshot. Reverse image search returned one individual visual match, an April 21 2022 post once again on r/facepalm:
Consequently, the tweet was no newer than April 2022. Using Twitter Advanced Search for “disability pride” and @somuchbeans returned no matching tweets.
The screenshot was shared to Facebook on July 3 2020, to Tumblr in September 2021, and to iFunny in December 2021; it seemed likely that @somuchbeans shared but later deleted the tweet due to its repeated virality.
A broader search returned a July 3 2023 tweet by @StynaLane, part of a lengthier thread. It appeared to be the first or most prominent iteration:
@SytnaLane’s thread consisted of 13 tweets in total, with a fourteenth tweet added in July 2023:
Overall, the viral first tweet made two discernible claims: that it was published during Disability Pride Month, and that disabled people living in the United STates with Medicaid “are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance.” In this context, “disabled people” appears to refer specifically to Americans entitled to and receiving disability benefits from the Social Security Administration — also known as Social Security Disability Insurance, or SSDI.
‘It’s Disability Pride Month’
Although the newest Reddit post above was shared in late August 2023, @StynaLane’s tweet was first shared in July 2020.
A resource published by the American Bar Association (ABA) confirmed that July is Disability Pride Month:
Disability Pride initially started as a day of celebration in 1990 — the year that the Americans with Disabilities Act (ADA) was signed into law. That same year, Boston held the first Disability Pride Day. The first official celebration of Disability Pride Month occurred in July 2015, which also marked the 25th anniversary of the ADA. Since then, cities across the country have celebrated disability pride month with parades and other festivities.
When the tweet was initially published, it was indeed in July — Disability Pride Month.
Medicaid in Brief
The second and more complex claim in the tweet was about restrictions purportedly placed on individuals who are eligible for and enrolled in Medicaid.
Medicaid is a government program that provides access to health care for adults and children with limited resources:
Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. Medicaid is administered by states, according to federal requirements. The program is funded jointly by states and the federal government.
Health policy research organization KFF (the Kaiser Family Foundation) published “10 Things to Know About Medicaid” in June 2023, and explained Medicaid as follows:
Medicaid is the primary program providing comprehensive coverage of health care and long-term services and supports to more than 90 million low-income people in the United States. The COVID-19 pandemic profoundly affected Medicaid spending and enrollment. In 2023, Medicaid programs are facing new challenges and millions of enrollees are at risk of losing coverage as states unwind the continuous enrollment provision that was put in place early in the pandemic to ensure stable coverage. The pandemic also focused policy attention on longstanding issues including: initiatives to reduce health disparities, expand access to care through the use of telehealth, improve access to behavioral health and home and community based services, and address workforce challenges.
The Biden Administration has efforts underway to help promote continuity of coverage, expand access, and has focused on closing the coverage gap in states that have not expanded Medicaid under the Affordable Care Act (ACA). Congressional Republicans have put forth proposals to reduce the deficit, limit federal spending for Medicaid, and impose work requirements in Medicaid. However, with divided government and recent passage of a bipartisan package to address the federal budget and increase the debt limit, there is unlikely to be much legislative activity on Medicaid in the next couple years …
A following section emphasized the importance of Medicaid benefits for a large number of people with disabilities under the age of 65 — i.e., people generally not yet eligible for Medicare coverage:
Medicaid is an entitlement, which means that individuals who meet eligibility requirements are guaranteed coverage. While Medicaid covers one in five people living in the United States, Medicaid is a particularly important source of coverage for certain populations. In 2021, Medicaid covered four in ten children, eight in ten children in poverty, one in six adults, and almost half of adults in poverty. Relative to White children and adults, Medicaid covers a higher share of Black, Hispanic, and American Indian American Native (AIAN) children and adults. Medicaid covers 43% of nonelderly, noninstitutionalized adults with disabilities, who are defined as having one or more difficulty related to hearing, vision, cognition, ambulation, self-care, or independent living[.]
The United States Department of Health and Human Services (HHS) contrasted Medicaid and Medicare, indicating that the latter does cover “some people” under 65:
Medicare is federal health insurance for people 65 or older, and some people under 65 with certain disabilities or conditions. A federal agency called the Centers for Medicare & Medicaid Services runs Medicare. Because it’s a federal program, Medicare has set standards for costs and coverage. This means a person’s Medicare coverage will be the same no matter what state they live in.
However, Medicaid — a state and federal program, not just federal — does not have an age requirement.
‘Disabled People in the US [Who Receive] Medicaid Are Not Allowed to Have More Than $2,000 in Money and Assets Combined, or Else We’ll Lose Our Often Life-Saving Health Insurance’
@StynaLane’s tweet was dated July 3 2020; on the same day, attorney Matthew Cortland retweeted it with additional commentary:
In the tweet and several threaded comments, Cortland analyzed the assertion and explained:
Hi friends, just want to expand on this a bit because it could dissuade folks who are eligible for Medicaid from seeking coverage.
The asset limit applies to Medicaid if Medicaid is going to be providing LTC (long term care), otherwise, there’s not an asset limit … Don’t misunderstand: it’s my position that there shouldn’t be an asset limit for Medicaid. But that’s a normative claim.
Under current law, it is factually incorrect, wrong, inaccurate, etc to say “disabled people in the US with Medicaid are not allowed to have more than $2,000 … What’s actually true is some formulation like “disabled people who rely on Medicaid to provide what Medicaid considers to be ‘long term care’ services (e.g. long term services and supports) are forced to apply for a kind of Medicaid that imposes a $2,000 asset limit”[.]
It’s also true that Medicaid is a federal-state partnership. What that means is that the feds set some rules, but states also have a lot flexibility – for example, using waiver programs, states can choose to provide HCBS/LTSS using different means testing requirements[.]
It isn’t always the case that the asset limit is $2k (it can vary not just from state to state, but from waiver program to waiver program in the same state) – and what “counts” as an asset can also vary.
LTSS (“long term services and supports”) “encompasses the broad range of paid & unpaid medical & personal care assistance that people may need–for several weeks, months, or years–when they experience difficulty completing self-care tasks…”
Cortland linked to a KFF “primer” on long-term care as it related to Medicaid, but it did not go into “asset limits,” or caps on assets. A Social Security Administration (SSA) resource described asset limits, but not in relation to Medicaid eligibility.
Much of the information about Medicaid eligibility and asset caps was state-specific, meaning that it was not necessarily consistent at the federal level. In July 2019, KFF published a report on Medicaid eligibility for “seniors and people with disabilities,” finding:
Pathways to Full Medicaid Eligibility Based on Old Age or Disability
SSI Beneficiaries
States generally must provide Medicaid to people who receive federal Supplemental Security Income (SSI) benefits. To be eligible for SSI, beneficiaries must have low incomes, limited assets, and an impaired ability to work at a substantial gainful level as a result of old age or significant disability. The SSI federal benefit rate is $750 per month for an individual and $1,125 for a couple in 2018, which [was] 74 percent of the federal poverty level (FPL). The effective SSI income limit is somewhat higher than 74% FPL in four states, due to state supplemental payments and/or additional income disregards: 80% FPL in Idaho, 83% FPL in New York and Wisconsin, and 87% FPL in Missouri … SSI beneficiaries also are subject to an asset limit of $2,000 for an individual and $3,000 for a couple … Two states (CT and NH) have a more restrictive asset limit ($1,600 and $1,500 for an individual, respectively), and three states (MN, MO, and ND) have a more generous asset limit ($3,000 for an individual) compared to the federal SSI rule ($2,000 for an individual).
Per KFF, a “federal SSI rule” occasionally varied by state, and capped assets at “$2,000 for an individual.” KFF issued a similar report in 2022, pointing out that states could offer alternative options:
States can choose to cover working people with disabilities whose income and/or assets exceed the limits for other eligibility pathways. This option enables people with disabilities to retain access to the medical and LTSS they need as their income increases. Medicaid often is especially important to working people with disabilities because private insurance typically does not cover all of the services and supports they need to live independently and to work. States can choose to apply an asset limit to this pathway. Eliminating asset limits, or increasing them beyond the SSI limit of $2,000 for an individual and $3,000 for a couple, recognizes that enrollees are likely to incur expenses related to work or community living and enables them to accrue some savings to meet future expenses. States also can choose to charge monthly premiums, usually on a sliding scale based on income.
KFF later described the $2,000 asset limit or cap as typically based on the SSI cap of $2,000 (several times):
States also can choose to apply an asset limit to medically needy pathways. The asset limit is typically the SSI amount of $2,000 for an individual and $3,000 for a couple, though it can be higher at state option … States also can choose to apply an asset limit to this pathway. The asset limit is typically the SSI amount of $2,000 for an individual and $3,000 for a couple, though it can be higher at state option.
A December 2021 Healio.com item, “‘Modest’ increase to Medicaid asset limits may boost eligibility for vulnerable seniors,” provided historical context about the introduction of asset limits:
… to receive Medicaid coverage, Medicare recipients must first undergo an asset test, which restricts eligibility by placing a limit on the value of assets held by the beneficiary. In most states, that limit was set in 1989 at $2,000 for an individual and $3,000 for a couple, and has remained unchanged ever since, according to the researchers.
Adjusted for inflation, that $2,000 in 1989 is now worth less than $900.
Citing research into asset limits and Medicaid, changes to asset limits was one of four things recommended by researchers to improve access to the program:
Increase the asset limit to $10,000 for individuals and $20,000 for couples, as proposed in the Supplemental Security Income Restoration Act of 2019. This would increase eligibility by 7.5% and again cover people who are more likely to be non-white and report having poorer health.
On August 17 2023, a long-term care facility published a blog post about California’s novel changes to, and eventual elimination of, Medicaid asset limits:
[California] is on the verge of becoming the first to completely eliminate its asset limit for all of its Medicaid programs. The Centers for Medicare & Medicaid Services approved California’s state plan amendment [in July 2023], calling it a “first of its kind.”
Assembly Bill 133 created a two-phased approach to eliminating the asset test for all non-modified adjusted gross income (Non-MAGI) Medi-Cal programs, including Medicare savings program and long-term care.
Phase I was implemented July 1, 2022, and increased the asset limit to $130,000 per individual and $65,000 for each additional family member. The previous limits were $2,000 for an individual, $3,000 for a couple and $150 for each additional family member.
Phase II will go into effect Jan. 1, 2024, and will eliminate the asset test entirely, allowing individuals to have a financial safety net for emergencies.
California’s Department of Health Care Services (DHCS) published a document about the asset limit changes in November 2021 [PDF], citing a then-current asset limit of “$2,000 per individual or $3,000 per couple.”
Finally, a VeryWellHealth article updated in May 2023 explained when and how Medicaid “asset tests” applied to benefits like Medicaid:
Two Categories of Medicaid Eligibility
Before the Affordable Care Act, Medicaid eligibility was based on how much money you earned and how much you owned, e.g., your income, your assets, and your net worth. After the law was enacted, however, eligibility was split into two distinct groups.
Some people continued to qualify for Medicaid the old fashioned way, while others qualify based on their modified adjusted gross income (MAGI) … Depending on which group you fall into, MAGI or non-MAGI, the government uses different factors to decide if you qualify for Medicaid.
In a subsequent section, the site explained that “non-MAGI Medicaid” recipients were subjected to an “asset test,” and that the $2,000/$3,000 cap was a “standard” based on Supplemental Security Income (SSI), “a means-tested program that provides cash payments to disabled children, disabled adults, and individuals aged 65 or older who are citizens or nationals of the United States”:
Medicaid and the Asset Test
When it comes to non-MAGI Medicaid eligibility, both your income and your assets come into play. Most of the government programs that qualify you for Medicaid, i.e., Medicare Savings Programs, use an asset test. SSI sets the standard.
If your income and assets are above a certain level, you will not qualify for the program. In 2023, the income limit is set at $2,742 per month and the asset limits at $2,000 for an individual.
MAGI Medicaid does not cover everything. Your assets come into play when it comes to Long-Term Services and Supports (LTSS), the part of Medicaid that pays for long-term care in a nursing home.
It then went into specific assets and exemptions (such as burial insurance or burial plots). With respect to cash on hand, the $2,000 figure was used as an example:
Your first $2,000 is yours and yours alone. Medicaid will only count any dollars above this amount. For example, if you have $2,500 in your bank account, only $500 will count toward your Medicaid qualifying assets.
Summary
On August 29 2023, an undated tweet about Disability Pride Month circulated, including a claim that disabled people in the U.S. with Medicaid “are not allowed to have more than $2,000 in money and assets combined” to continue receiving Medicaid benefits. The tweet was published in July 2020, during Disability Pride Month.
As for the claim about disabled people being subjected to an asset limit of $2,000, it had to do with non-MAGI Medicaid eligibility — the form of Medicaid available to disabled adults under the age of 65. As of August 2023, California was in the process of eliminating Medicaid asset tests. However, the limit of $2,000 for a person and $3,000 for a couple was referenced in most resources about Medicaid eligibility, disability, and assets.
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | Reddit
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | Reddit
- disability pride (from:somuchbeans) | Twitter Advanced Search
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | Facebook
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | Tumblr
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | iFunny
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | Twitter
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | Twitter Unroller
- It’s disability pride month, and did you know disabled people in the US with Medicaid are not allowed to have more than $2,000 in money and assets combined, or else we’ll lose our often life-saving health insurance? ???? | Twitter
- Disability Pride Month
- Medicaid | Wikipedia
- 10 Things to Know About Medicaid | KFF
- What’s the difference between Medicare and Medicaid? | HHS
- The asset limit applies to Medicaid if Medicaid is going to be providing LTC (long term care), otherwise, there's not an asset limit | Matthew Cortland/Twitter
- Medicaid and Long-Term Services and Supports: A Primer | KFF
- Social Security asset limits | SSA.gov
- Medicaid Financial Eligibility for Seniors and People with Disabilities: Findings from a 50-State Survey
- Medicaid Financial Eligibility in Pathways Based on Old Age or Disability in 2022: Findings from a 50-State Survey | KFF
- 'Modest' increase to Medicaid asset limits may boost eligibility for vulnerable seniors
- State becomes first to strip Medicaid asset limit
- Medicaid asset limits | California Department of Health Care Services
- Medicaid Eligibility: MAGI and Your Assets